Immunity
Immunity means being protected from something and being unaffected or not bothered by it. Let’s say you have immunity to heat – this means heat can’t bother you whatsoever – walking up to hot molten lava would be no different than walking up to normal water.
- Immunity to a disease is achieved through the presence of antibodies to that disease in a person’s system.
- Antibodies are proteins produced by the body to neutralize or destroy toxins or disease-carrying organisms. Antibodies are disease-specific. For example, a measles antibody will protect a person who is exposed to measles disease but will have no effect if he or she is exposed to mumps.
- Our immune system protects us and helps fight off disease. Many microbes and viruses can cause disease and are termed pathogens. With all these pathogens around, why aren’t we sick every single moment? The answer is our immune system gives us different types of immunity to protect us from disease.
Types Of Immunity
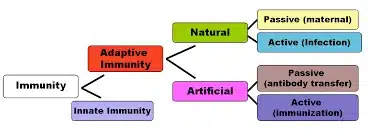
There are two main types of immunity:
- Innate, also called natural or inherited,
- Adaptive, also called acquired immunity
Innate Immunity
- Plants and animals have what is called innate immunity.
- Innate immunity is the first line of defense against pathogens.
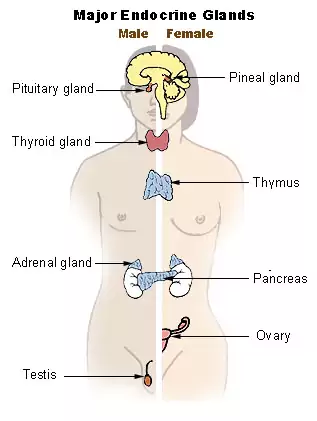
- It involves several cell types, proteins, and even an organ.
- The organ involved is your skin. Yes, skin is part of the first line of defense. It protects you and prevents pathogens from getting inside your body.
So, what are some ways a pathogen gets inside?
- Air, food, or a break in the skin are some ways a pathogen enters. A pathogen entering through food or air has mucus to go through. The mucosal surfaces prevent pathogens from attaching to cells and causing disease. A pathogen getting through skin and mucus will have to deal with several types of cells including phagocytes, eating cells, and natural killer (NK) cells before it can cause disease.
- Pathogens have warning flags on their surface that say: ‘I don’t belong here’. Neutrophils, macrophages, and dendritic cells are all phagocytes. They recognize the warning flag, attack the pathogen, and eat it – a process known as phagocytosis.
- If a pathogen is too big for one cell alone, several cells attack at once. NK cells on the other hand, identify infected cells (host cells) and activate the host cell’s death receptor pathway or give the cell a lethal injection (injecting enzymes that degrade proteins).
- Host cells even try to fight back by turning off machinery that would help the pathogen and sending out distress signals.
- If pathogens make it through all this, it’s time for adaptive immunity to step in, and they do this with the help of dendritic cells.
Adaptive Immunity
- Adaptive immunity works slower than innate and is more specific.
- Adaptive immunity is an immunity that occurs after exposure to an antigen either from a pathogen or a vaccination.
- This part of the immune system is activated when the innate immune response is insufficient to control an infection.
There are two types of adaptive immunity: Active immunity and Passive immunity.
Active Immunity
- Active immunity results when exposure to a disease organism triggers the immune system to produce antibodies to that disease.
- Exposure to the disease organism can occur through infection with the actual disease (resulting in natural immunity), or the introduction of a killed or weakened form of the disease organism through vaccination (vaccine-induced immunity).
- Either way, if an immune person comes into contact with that disease in the future, their immune system will recognize it and immediately produce the antibodies needed to fight it.
- Active immunity is long-lasting, and sometimes life-long.
- Active immunity involves two types of white blood cells – T-cells and B-cells. Dendritic cells, after they have eaten and digested the pathogen, present the pathogen pieces to T-cells, which activate (turn on) the T-cells.
Passive Immunity
- Passive immunity occurs when antibodies are passed from one person to another, as through transfusion for example. Today plasma therapy is in news. In plasma therapy, the antibody is transfused from a recovered person to a diseased one. This is an example of creating adaptive immunity in the diseased person.
- Passive immunity is provided when a person is given antibodies to a disease rather than producing them through his or her own immune system.
- A newborn baby acquires passive immunity from its mother through the placenta. A person can also get passive immunity through antibody-containing blood products such as immune globulin, which may be given when immediate protection from a specific disease is needed. This is the major advantage to passive immunity; protection is immediate, whereas active immunity takes time (usually several weeks) to develop.
- However, passive immunity lasts only for a few weeks or months. Only active immunity is long-lasting.
How does the immune system respond to a coronavirus attack?
- A cascade of viral particles enters the body through the nose, eyes, or mouth. Breathing carries some of these particles to the lower respiratory tract where the spike proteins of the coronavirus, acting as a key, lock into epithelial cells that line the respiratory tract as well as those in the air sacs in the lungs.
- COVID-19 is able to stay undetected longer than many flu or coronaviruses and its spike proteins are able to gain entry by unlocking the ACE2 protein on the lung cells. Once in, they hijack the cell’s machinery, replicate and multiply and infect adjoining cells.
- Like the defining ACE2 proteins on the epithelial cells, viruses too have a tell-tale signature on their surface called antigens, and spotting these is what kicks the immune system into action by producing antibodies.
- The signals they generate trigger another class of chemicals — cytokines and chemokines — and they alert the immune system to send an array of different kinds of cells that specialize in destroying viral particles. However, these cytokines and chemokines trigger inflammation in the cells.
- In the nose and upper regions of the respiratory system, this inflammation produces mucus and a runny nose to trap viral particles and prevent their ingress. This also triggers sneezes to expel them.
- When the sinuses are inflamed we get a headache and the general stuffiness that we associate with a cold. When a gland called the hypothalamus is inflamed, it results in a fever.
- However, in the case of COVID-19, the virus seems better at penetrating deeper. The inflammation triggers a fluid build-up in the lungs. The fluids also contain the residue of a host of specialized cells — including T cells — that carpet bomb and damage many of the body’s own cells as well as the viral particles.
- It is in expelling this fluid that a dry cough, characteristic of the coronavirus infection, begins. As more air sacs are infected, the lungs find it harder to perform their core job of extracting oxygen from the air, and eventually, this aggravates breathlessness.
Why are some infections mild and others life-threatening?
- Depending on the degree of infection in the lungs, the inflammation and the fluid build-up can lead to pneumonia. A patient will require hospitalization to treat the breathlessness and ventilator support to artificially provide oxygen if the condition worsens.
- However, massive levels of cytokines can cause extensive lung damage and a condition called Acute Respiratory Distress Syndrome. The unsustainable cytokine storm can cause organ damage far beyond the lungs and spread to the kidneys as well as the heart.
- If the infection is acute, it can also lead to a depletion of the frontline white blood corpuscles tasked with fighting the infection and making the body vulnerable to other secondary infections, which may lead to death.
How have the elderly reacted to the virus?
- The elderly, especially those with existing conditions such as diabetes and cardiovascular disease, already have an inherent malfunctioning immune system.
- In many ways, it is the reaction of the body is trying to combat the virus that ends up being suicidal.
- The different kinds of drugs, whether it is hydroxychloroquine or anti-HIV drugs, deployed to treat serious COVID-19 infection, also work in some way to moderate the immune system’s aggressive defense.
Herd immunity
- Herd immunity is when a virus can no longer spread easily because enough people are immune to it. That lowers the chances of the virus jumping from person to person and reaching those who haven’t been infected yet.
- People can become immune to certain viruses after surviving an infection or being vaccinated. Typically, at least 70% of a population must be immune to achieve herd immunity. But how long immunity lasts varies depending on the virus, and it’s not yet known how long COVID-19 survivors might have that protection.
- The premise is that if a certain percentage is immune, members of that group can no longer infect another person. This breaks the chain of infection through the community (“herd”) and prevents it from reaching those who are the most vulnerable.
For more articles on sci-tech, click here.
Also refer :