What are T cells and why are they important?
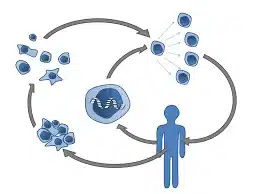
For your immune system to fight off any kind of invader, such as a virus, you need a kind of white blood cell called a B cell, which makes antibodies, and a similar-looking white blood cell called a T cell.
T cells can play different roles. They can act as “killer cells”, attacking cells which have been infected with a virus or another kind of pathogen, or they can act as “helper cells” by supporting B cells to produce antibodies.
T-cells are a type of lymphocyte (a type of white blood immune cell) that are involved in bringing about an adaptive immune response. T cells are so-called ‘T- ‘cells because they develop in the thymus. There are two main types of T cells: CD8+ ‘killer’ or ‘cytotoxic’ T cells (Tc cells), and CD4+ ‘helper’ T cells (Th cells).
CD8+ TC cells can directly kill pathogen-infected cells as well as recruiting other immune cells by cytokine signaling to ensure a robust immune response is carried out. CD8+ TC cells express T cell receptors (TCRs) which can recognize specific pathogenic (viral) or foreign antigens.
Any cell infected by a pathogen displays the antigen on its cell surface through class I MHC, to which specific CD8+ TC cells can bind via their TCR. This binding activates an immature CD8+ TC cell to enable it to carry out its cytotoxic (cell-killing) role.
CD4+ Th cells on the other hand can recruit B-cells (another lymphocyte that produces antibodies) amongst other cells by recognizing antigens displayed by class II MHC molecules binding to their specific TCR. Also, the cytokines released by CD4+ Th cells can allow B-cell antibody class switching as well as the activation and proliferation of CD8+ TC cells.
More info about T-cell immunity
When people become unwell from COVID-19, we know that their white blood cell count goes down a lot, but it’s their T cells that are particularly impacted. We don’t know yet whether the T cells actually die, or whether they’ve just moved somewhere else. One confusing thing is that, with COVID-19, you can have bursts of T cells that are both activated and exhausted-looking and it’s difficult to explain why this is.
Antibodies can only latch onto and help destroy pathogens outside cells and may also occasionally, paradoxically, enhance a pathogen’s ability to infect cell instead by antibody dependent ”enhancement” or ADE. It is only the T-cell that can cleverly sense and destroy pathogens inside infected cells using “sensors” which detect foreign protein fragments.
Why are some people unable to mount a good protective T-cell response?
When a T cell is exposed to a foreign pathogen, it extends a signalling device or ‘antenna’ known as a vitamin D receptor, with which it searches for vitamin D, and if there is an inadequate vitamin D level, “they won’t even begin to mobilize.” In other words, adequate vitamin D is critically important for the activation of T-cells from their inactive naive state. The question of whether T-cells might also need a continuing supply of vitamin D to prevent the T-cell exhaustion and apoptosis observed in some serious COVID-19 cases deserves further research.
High levels of vitamin D are also critical for first line immune defences including physical mucosal defences, human antiviral production, modulating cytokines, reducing blood clotting and a whole host of other important immune system functions . The obese, diabetics and people of BAME origin are far more deficient in vitamin D and men have lower levels than women .
Japanese have very high vitamin D levels of over 30 ng/ml in 95% of the active elderly. By comparison, UK average levels are below 20ng/ml. Vitamin D is made in the skin from the action of UV sunlight, food usually being a poor source, but the Japanese diet includes unusually high levels. Sunny countries near the equator (e.g. Nigeria, Singapore, Sri Lanka) also have very low COVID related deaths.
In summary, a vast majority of COVID-19 patients develop an immune response against SARS-CoV-2 with the activation of T-cells to the spike-protein of the virus. By recognizing the spike-protein specifically the receptor-binding domain – which is the most effective site for neutralizing antibodies – a robust immune response can be mounted and may remain protective for future infections.
Also refer :